Location of ambulances for Cucuta's emergency medical system
DOI:
https://doi.org/10.17981/ingecuc.20.1.2024.11Keywords:
Pre-hospital care, operations research, hospital logistics, optimization, Emergency Medical ServicesAbstract
Introduction. The location of ambulance bases is a strategic decision in the emergency medical system (EMS), which impacts the response time and the probability of saving lives or leaving sequelae in patients who suffer traffic accidents or disease crises.
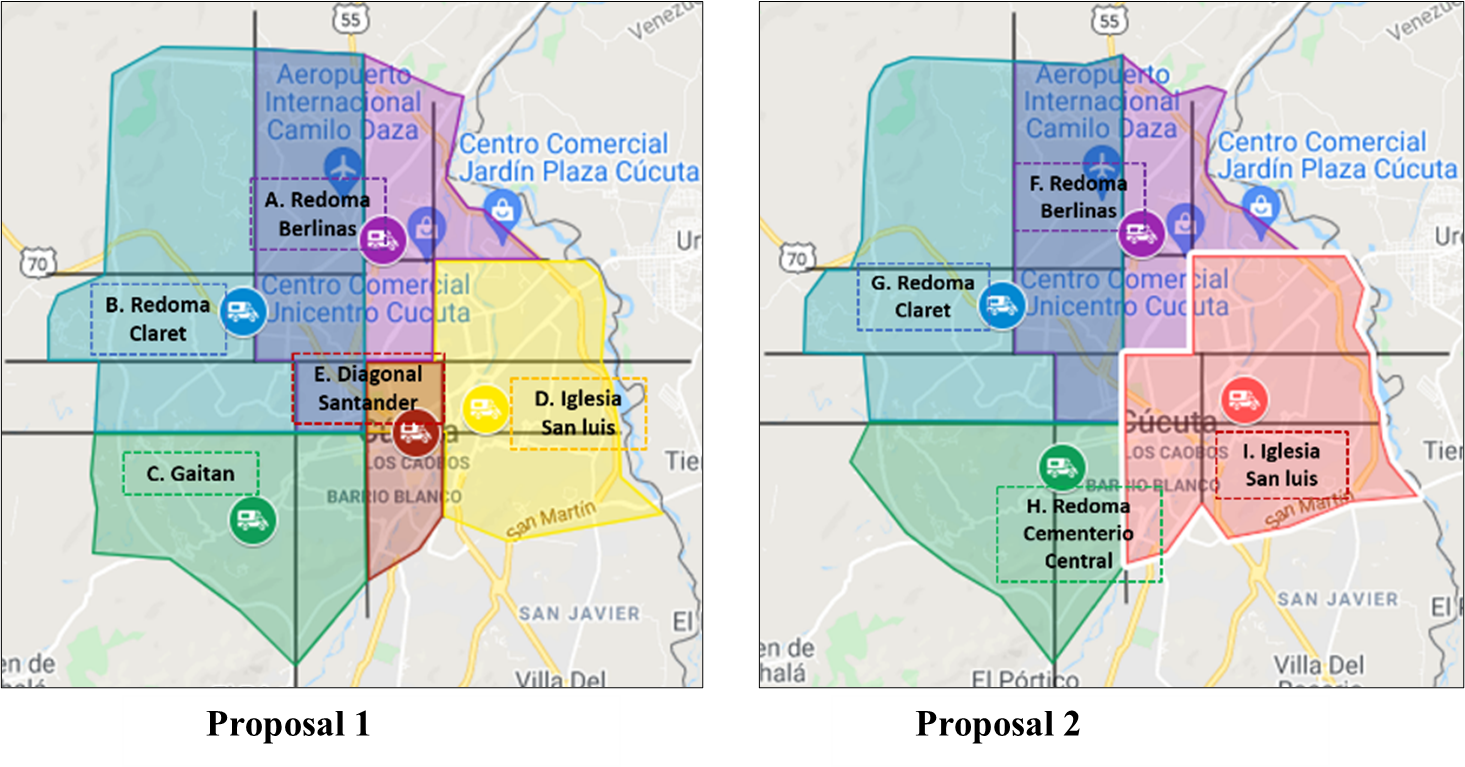
Objective. The research proposed the location of ambulance bases for EMS to improve the timeliness of pre-hospital care in Cucuta.
Methodology. First, this research used the center of gravity method to segment the city into sub-quadrants and determine alternative locations. Second, the location factors scoring method was employed to evaluate alternative sites. Third, an integer linear programming model was designed to select the optimal location of ambulances in Cucuta that minimizes the number of ambulance bases to care for traffic accidents in a response time of 8 minutes or less. Finally, a code was developed using Python 3.8.2 and the Google Maps Direction API web service to determine the response times.
Results. This paper proposed two optimal location alternatives, reducing the average response time from 10.96 minutes to 5.39 and 5.72, an improvement of 50.82% and 47.81%, respectively. In addition, the patients cared for in a response time of 8 minutes or less would increase to 85.19% and 78.84%, improving the 30.82% of the current situation.
Conclusions. The second location proposal, which considered four bases, was suggested because it would facilitate EMS control and logistics management of ambulances and enhance the timeliness of pre-hospital care in Cúcuta.
Downloads
References
M. García, J. Navarrete, N. Soracá, C. Montoya, and D. Barrera, “Diseño de una técnica de solución para la localización de ambulancias en Bogotá,” Pontificia Universidad Javeriana, 2019.
J. Cho and Y. Yoon, “GIS-Based Analysis on Vulnerability of Ambulance Response Coverage to Traffic Condition: A Case Study of Seoul,” in IEEE Conference on Intelligent Transportation Systems, Proceedings, ITSC, 2015, pp. 1402–1407. doi: 10.1109/ITSC.2015.230.
M. H. Azizan, C. S. Lim, W. A. L. W. M. Hatta, T. L. Go, and S. S. Teoh, “Simulation of Emergency Medical Services delivery performance based on real map,” Int. J. Eng. Technol., vol. 5, no. 3, pp. 2620–2627, 2013.
T. Ferrari et al., “Analysis of the Location of Rescue Ambulance Dispatch Bases: A Case Study in Rio de Janeiro, Brazil,” Geogr. Anal., vol. 50, no. 4, pp. 397–421, 2018, doi: 10.1111/gean.12172.
H. Leknes, E. S. Aartun, H. Andersson, M. Christiansen, and T. A. Granberg, “Strategic ambulance location for heterogeneous regions,” Eur. J. Oper. Res., vol. 260, no. 1, pp. 122–133, 2017, doi: 10.1016/j.ejor.2016.12.020.
P. Zapata and M. Baldoquin, “Vehicle location models for Emergency Medical Services. An application for a Colombian company,” Rev. EIA, vol. 15, no. 29, pp. 31–46, 2018, doi: 10.24050/reia.v15i29.1211.
H. Toro-Díaz, M. E. Mayorga, S. Chanta, and L. A. McLay, “Joint location and dispatching decisions for Emergency Medical Services,” Comput. Ind. Eng., vol. 64, no. 4, pp. 917–928, 2013, doi: 10.1016/j.cie.2013.01.002.
M. Gendreau, G. Laporte, and F. Semet, “Solving an ambulance location model by tabu search,” Locat. Sci., vol. 5, no. 2, pp. 75–88, 1997, doi: https://doi.org/10.1016/S0966-8349(97)00015-6.
M. H. Azizan, C. S. Lim, W. A. L. W. M. Hatta, and L. C. Gan, “Application of OpenStreetMap data in ambulance location problem,” Proc. - 2012 4th Int. Conf. Comput. Intell. Commun. Syst. Networks, CICSyN 2012, pp. 321–325, 2012, doi: 10.1109/CICSyN.2012.66.
N. Velásquez, S. Naranjo, and G. González, “Indicadores de Atención Pre Hospitalaria para incidentes viales en Colombia,” Rev. Fac. Nac. Salud Pública, vol. 35, no. 3, pp. 410–419, 2017, doi: 10.17533/udea.rfnsp.v35n3a11.
S. Menéndez, N. Navarrete, and A. Paz, “Tiempos de respuesta del sistema prehospitalario en pacientes con sospecha diagnóstica de ataque cerebral en Bogotá durante los años 2013 y 2014..,” Acta Neurológica Colomb., vol. 33, no. 3, pp. 135–141, 2017, doi: 10.22379/24224022147.
E. C. Jauch et al., “Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association,” Stroke, vol. 44, no. 3, pp. 870–947, 2013, doi: 10.1161/STR.0b013e318284056a.
V. Duque, T. Henao, N. Pérez, and C. Pérez, “Tiempo de respueta de atención pre-hospitalaria en accidentes motociclísticos VS la satisfacción objetiva del paciente frente a los procedimientos,” Universidad CES, 2013.
D. Gonzáles, “Una solución al sistema de respuesta de emergencias de Antioquia a la demora en el tiempo de traslado de los pacientes,” Universidad CES, 2016.
L. Aboueljinane, E. Sahin, Z. Jemai, and J. Marty, “A simulation study to improve the performance of an emergency medical service: Application to the French Val-de-Marne department,” Simul. Model. Pract. Theory, vol. 47, pp. 46–59, 2014, doi: 10.1016/j.simpat.2014.05.007.
S. M. Gholami-Zanjani, M. S. Pishvaee, and S. A. Torabi, “OR Models for Emergency Medical Service (EMS) Management,” in Operations Research Applications in Health Care Management, Springer, Cham., 2018, pp. 395–421.
R. Aringhieri, M. E. Bruni, S. Khodaparasti, and J. T. van Essen, “Emergency medical services and beyond: Addressing new challenges through a wide literature review,” Comput. Oper. Res., vol. 78, pp. 349–368, 2017, doi: 10.1016/j.cor.2016.09.016.
Y. Kergosien, V. Bélanger, P. Soriano, M. Gendreau, and A. Ruiz, “A generic and flexible simulation-based analysis tool for EMS management,” Int. J. Prod. Res., vol. 53, no. 24, pp. 7299–7316, 2015, doi: 10.1080/00207543.2015.1037405.
M. Reuter-Oppermann, P. L. van den Berg, and J. L. Vile, “Logistics for Emergency Medical Service systems,” Heal. Syst., no. October, 2017, doi: 10.1057/s41306-017-0023-x.
H. Montenegro, “Modelo cuantitativo para la localización de Ambulancias de Gestión Sanitaria y su impacto en los tiempos de arribo, coordinadas por el Centro Local ECU911 Macas dentro de la provincia de Morona Santiago,” Universidad Técnica De Ambato, 2017.
P. L. Van Den Berg, P. Fiskerstrand, K. Aardal, J. Einerkjær, T. Thoresen, and J. Røislien, “Improving ambulance coverage in a mixed urban-rural region in Norway using mathematical modeling,” PLoS One, vol. 14, no. 4, pp. 1–14, 2019, doi: 10.1371/journal.pone.0215385.
M. Liu, D. Yang, and F. Hao, “Optimization for the Locations of Ambulances under Two-Stage Life Rescue in the Emergency Medical Service: A Case Study in Shanghai, China,” Math. Probl. Eng., vol. 2017, 2017, doi: 10.1155/2017/1830480.
J. M. Holguín, D. A. Escobar, and J. A. Tamayo, “Servicio de urgencias versus infraestructura de transporte. Un análisis de accesibilidad enfocado en las desigualdades sociales. Caso de estudio: Manizales, Colombia,” Inf. Tecnol., vol. 28, no. 2, pp. 125–134, 2017, doi: 10.4067/S0718-07642017000200014.
K. Holtermann et al., Desarrollo de sistemas de emergencias médicos: experiencia de los Estados Unidos de América para países en desarrollo. Washington, 2003.
M. de S. y P. S. MSPS, “Resolución 0926 del 30 de marzo de 2017. Por la cual se reglamenta el desarrollo y operación del Sistema de Emergencias Médicas.,” no. 30 marzo 2017. 2017.
C. de la república de C. CRC, “Ley No. 1438 de 2011. Por medio de la cual se reforma el sistema general de seguridad social en salud y se dictan otras disposiciones.” p. 51, 2011.
E. Segura, R. Carmona, I. Sangermán, and A. Lozano, “Localización de ambulancias utilizando programación lineal: caso UNAM,” in Congreso Latino-Iberoamericano de Investigación Operativa (CLAIO), P. Z. Rios-Mercado, Ed., Monterreey, 2014, pp. 351–358.
J. Villegas, C. Castañeda, and K. Blandón, “Mejoramiento de la localización de ambulancias de atención prehospitalaria en Medellín (Colombia) con modelos de optimización,” in Congreso Latino-Iberoamericano de Investigación Operativa, Rio de Janeiro, 2012, pp. 731–742.
J. J. Leuro, “Aplicación de un modelo de localización de unidades tácticas de atención de emergencias (ambulancias ) en la ciudad de Bogotá,” Rev. Entérese Boletín Científico Univ., no. 33, pp. 44–56, 2012.
A. Rojas, L. Alvarez, and J. Parra, “Diseño metodológico para la ubicación de ambulancias del sector de atención prehospitalaria en Bogotá D.C.,” Rev. Ing. Ind., vol. 6, no. 1, pp. 77–94, 2007.
R. Chase, R. Jacobs, and N. Aquilano, Administración de operaiones. Producción y cadenas de suministros, Duodécima. México: Mc Graw Hill, 2009.
C. Toregas, R. Swain, C. ReVelle, and L. Bergman, “The Location of Emergency Service Facilities,” Oper. Res., vol. 19, no. 6, pp. 1363–1373, 1971, doi: 10.1287/opre.19.6.1363.
J. Bezanson, S. Karpinski, V. B. Shah, and A. Edelman, “Julia: a fast dynamic language for technical computing.” arXiv:1209.5145, pp. 2–27, 2012. doi: https://doi.org/10.48550/arXiv.1209.5145.
L. A. C. G. Andrade and C. B. Cunha, “An ABC heuristic for optimizing moveable ambulance station location and vehicle repositioning for the city of São Paulo,” Int. Trans. Oper. Res., vol. 22, no. 3, pp. 473–501, 2015, doi: 10.1111/itor.12160.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 INGE CUC

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Published papers are the exclusive responsibility of their authors and do not necessary reflect the opinions of the editorial committee.
INGE CUC Journal respects the moral rights of its authors, whom must cede the editorial committee the patrimonial rights of the published material. In turn, the authors inform that the current work is unpublished and has not been previously published.
All articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.


 English
English
 Español (España)
Español (España)