Heart Rate Monitoring Applications on Open Source Platforms: A Review
DOI:
https://doi.org/10.17981/bilo.2.2.2020.1Keywords:
Open Source, E-healt, biomedicine, heart rateAbstract
Introduction: Technological developments that are implemented in open source platforms have grown considerably in the last decade, offering easy-to-develop, flexible and low-cost solutions. In the case of biomedical applications developed on Open Source platforms, heart rate monitoring is one of the most developed applications.
Objective: this document presents a systematic review of the literature, in which current developments in Heart Rate Monitoring Systems (SMFC) on Open Source platforms are analyzed. The most significant developments and commonly used platforms are identified.
Method: A systematic review of the Cochrane-type literature is carried out.
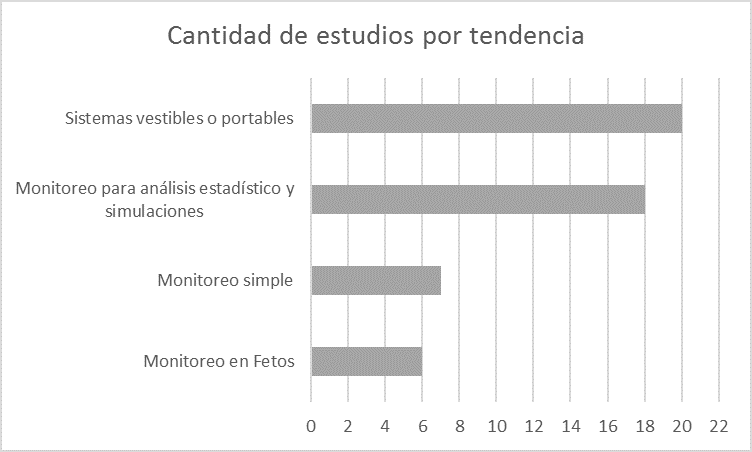
Results: The trends in research about heart rate monitoring systems using Open Source platforms are presented.
Conclusions: there is a great development of applications that involve heart rate monitoring. However, his study is not finished. Since, with the large amount of data available thanks to these applications, it is still possible to deepen the implementation of statistical studies.
Downloads
References
J. A. Merlo Vega, Ecosistemas del acceso abierto, 1era ed. Salamanca, España: Aqui La Fuente, 2018.
C. Park and B. Lee, “Real-time estimation of respiratory rate from a photoplethysmogram using an adaptive lattice notch filter,” Biomed. Eng. Online, vol. 13, no. 1, 2014.
L. L. Hamilton, “An instant heart rate monitor.,” J. Appl. Physiol., vol. 24, no. 4, pp. 585–587, 1968.
Comisión Europea, “EUR-Lex - 32017D0863 - ES - EUR-Lex,” 2017. [Online]. Available: https://eur-lex.europa.eu/legal-content/ES/TXT/?qid=1562189303314&uri=CELEX:32017D0863. [Accessed: 03-Jul-2019].
OMS, “Enfermedad pulmonar obstructiva crónica (EPOC),” 2017. [Online]. Available: https://www.who.int/es/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). [Accessed: 03-Jul-2019].
S. Shafi, S. Harish, S. Tej, and P. Raj, “An efficient and low cost real time heart rate monitoring and alerting system using virtual instrumentation,” Int. J. Recent Technol. Eng., vol. 8, no. 1, pp. 325–328, 2019.
J. P. Gisbert, “¿ Cómo realizar , evaluar y utilizar revisiones sistemáticas y metaanálisis ?,” vol. 27, no. 3, pp. 129–149, 2004.
A. Page, T. Soyata, J.-P. Couderc, and M. Aktas, “An open source ECG clock generator for visualization of long-term cardiac monitoring data,” IEEE Access, vol. 3, pp. 2704–2714, 2015.
J.-C. Edelmann, D. Mair, D. Ziesel, M. Burtscher, and T. Ussmueller, “An ECG simulator with a novel ECG profile for physiological signals,” J. Med. Eng. Technol., vol. 42, no. 7, pp. 501–509, 2018.
C. Funck-Brentano et al., “Evaluation of the effects on the QT-interval of 4 artemisinin-based combination therapies with a correction-free and heart rate-free method,” Sci. Rep., vol. 9, no. 1, 2019.
M. Siahkouhian and D. Khodadadi, “Narita target heart rate equation underestimates the predicted adequate exercise level in sedentary young boys,” Asian J. Sports Med., vol. 4, no. 3, pp. 175–180, 2013.
Z. S. Cicone, O. A. Sinelnikov, and M. R. Esco, “Age-predicted maximal heart rate equations are inaccurate for use in youth male soccer players,” Pediatr. Exerc. Sci., vol. 30, no. 4, pp. 495–499, 2018.
I. García-Magariño and I. Plaza, “ABS-MindHeart: An agent based simulator of the influence of mindfulness programs on heart rate variability,” J. Comput. Sci., vol. 19, pp. 11–20, 2017.
A. N. Vest et al., “An open source benchmarked toolbox for cardiovascular waveform and interval analysis,” Physiol. Meas., vol. 39, no. 10, 2018.
M. Varanini, G. Tartarisco, L. Billeci, A. Macerata, G. Pioggia, and R. Balocchi, “An efficient unsupervised fetal QRS complex detection from abdominal maternal ECG,” Physiol. Meas., vol. 35, no. 8, pp. 1607–1619, 2014.
P. M. Pinto Silva and J. P. Silva Cunha, “SenseMyHeart: A cloud service and API for wearable heart monitors,” in 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBC 2015, 2015, vol. 2015-Novem, pp. 4986–4989.
F. B. A. Schneider, A. S. de Melo, R. V Andreão, and R. F. Dalvi, “Alternative class III distributed polysomnography system,” Res. Biomed. Eng., vol. 34, no. 2, pp. 127–137, 2018.
J. Gonzalez, E. Galvis, and C. Velandia, “Implementation of real-time filter using an open-source platform oriented to R-wave detection,” in 21st Symposium on Signal Processing, Images and Artificial Vision, STSIVA 2016, 2016.
A. Lichtman, R. Uzsák, M. Svetlák, and P. Fuchs, “A smart electrocardiogram monitoring system on android,” in 2018 International Conference on New Trends in Signal Processing, NTSP 2018, 2018, pp. 94–98.
G. D. Clifford et al., “A scalable mHealth system for noncommunicable disease management,” in 4th IEEE Global Humanitarian Technology Conference, GHTC 2014, 2014, pp. 41–48.
B. B. Rekha, A. Kandaswamy, and V. M. Mitha, “Embedded realization of a real time Heart Rate Variability logger for at-home sleep studies,” in 2015 IEEE Workshop on Computational Intelligence: Theories, Applications and Future Directions, WCI 2015, 2016.
M. Cieslak et al., “Quantifying rapid changes in cardiovascular state with a moving ensemble average,” Psychophysiology, vol. 55, no. 4, 2018.
J. R. Balbin et al., “Development of scientific system for assessment of post-traumatic stress disorder patients using physiological sensors and feature extraction for emotional state analysis,” in 9th IEEE International Conference on Humanoid, Nanotechnology, Information Technology, Communication and Control, Environment and Management, HNICEM 2017, 2018, vol. 2018-Janua, pp. 1–6.
PhysioNet.org, “PhysioNet.” [Online]. Available: https://physionet.org/. [Accessed: 05-Jul-2019].
R. Abbas, A. J. Hussain, D. Al-Jumeily, T. Baker, and A. Khattak, “Classification of Foetal Distress and Hypoxia Using Machine Learning Approaches,” 14th International Conference on Intelligent Computing, ICIC 2018, vol. 10956 LNAI. Springer Verlag, Department of Computer Science, Liverpool John Moores University, Liverpool, L33AF, United Kingdom, pp. 767–776, 2018.
L. Wang and X. Zhou, “Detection of congestive heart failure based on LSTM-based deep network via short-term RR intervals,” Sensors (Switzerland), vol. 19, no. 7, 2019.
N. Vila Blanco, L. Rodríguez-Liñares, P. Cuesta, M. J. Lado, A. J. Méndez, and X. A. Vila, “gVARVI: A graphical software tool for the acquisition of the heart rate in response to external stimuli,” Comput. Methods Programs Biomed., vol. 132, pp. 197–205, 2016.
J. Wang, W. Chen, and G. Hou, “Parallel computing method for HRV time-domain based on GPU,” 15th International Conference on Algorithms and Architectures for Parallel Processing, ICA3PP 2015, vol. 9529. Springer Verlag, School of Software Technology, Dalian University of Technology, Economic and Technological Development Zone, Dalian, 116600, China, pp. 434–443, 2015.
S. K. Nair, H. Kasturiwale, and S. N. Kale, “Quantification of heart rate variability for health analysis,” in International Conference and Workshop on Electronics and Telecommunication Engineering, ICWET 2016, 2016, vol. 2016, no. CP700, pp. 178–183.
J. Gierałtowski, K. Ciuchciński, I. Grzegorczyk, K. Kos̈na, M. Soliński, and P. Podziemski, “RS slope detection algorithm for extraction of heart rate from noisy, multimodal recordings,” Physiol. Meas., vol. 36, no. 8, pp. 1743–1761, 2015.
J. Behar, A. Johnson, G. D. Clifford, and J. Oster, “A comparison of single channel fetal ecg extraction methods,” Ann. Biomed. Eng., vol. 42, no. 6, pp. 1340–1353, 2014.
J. Behar, F. Andreotti, S. Zaunseder, Q. Li, J. Oster, and G. D. Clifford, “An ECG simulator for generating maternal-foetal activity mixtures on abdominal ECG recordings,” Physiol. Meas., vol. 35, no. 8, pp. 1537–1550, 2014.
F. Andreotti, F. Graser, H. Malberg, and S. Zaunseder, “Non-invasive Fetal ECG Signal Quality Assessment for Multichannel Heart Rate Estimation,” IEEE Trans. Biomed. Eng., vol. 64, no. 12, pp. 2793–2802, 2017.
J. A. Behar et al., “PhysioZoo: A novel open access platform for heart rate variability analysis of mammalian electrocardiographic data,” Front. Physiol., vol. 9, no. OCT, 2018.
D. Yu, D. Du, H. Yang, and Y. Tu, “Parallel computing simulation of electrical excitation and conduction in the 3D human heart,” in 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBC 2014, 2014, pp. 4315–4319.
M. S. Mahmud, H. Fang, and H. Wang, “An Integrated Wearable Sensor for Unobtrusive Continuous Measurement of Autonomic Nervous System,” IEEE Internet Things J., vol. 6, no. 1, pp. 1104–1113, 2019.
L. Stanciu and A. Mucioniu, “Multifunctional portable equipment for medical and biometric applications,” in 5th IEEE International Conference on E-Health and Bioengineering, EHB 2015, 2016.
A. Sánchez Comas, A. Troncoso Palacio, S. Troncoso Mendoza, and D. Neira Rodado, “Application of taguchi experimental design for identication of factors influence over 3D printing time with fused deposition modeling,” IJMSOR, vol. 1, no. 1, pp. 43–48, 2016.

 English
English
 Español (España)
Español (España)
